AI: Finding the Fraud Needle in the Big Data Haystack
Artificial Intelligence approach used against fraud, waste, and abuse not only uncovers specific instances, but often provides additional insights. Fraud and abuse are on the rise in the health care industry’s rapidly advancing technology.
FWA can occur anywhere within the health care system, pharmacies or members engaged in myriad schemes like, Phantom pharmacies and ID theft, Diabetic test strip resales, Telemedicine and online dispensing of prescription meds, Compound prescription fraud.
It creates new avenues for criminals’ illicit exploits and enables them to operate with relative ease and anonymity. Powerful capabilities make fraud investigators’ jobs easier finding those fraud “needles” in the big data “haystack.
AI has become a viable option for most companies. It can run on low-cost servers instead of supercomputers, as was required in years past. Some pharmacy benefit managers (PBMs) have deployed anti-fraud analytics platforms to help their health plans wage battle with fraudsters.
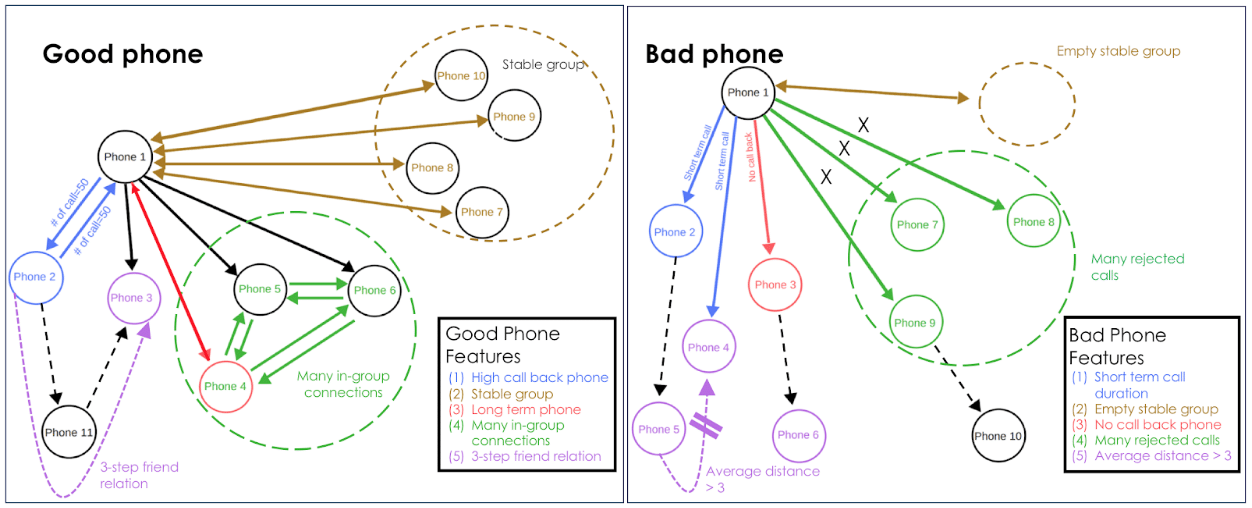
AI spotlights potential instances of fraud, saving investigators from much of the more tedious, time-consuming work and helping optimize their investigative resources. In this systematic AI approach is used against FWA, benefits managers not only uncover specific instances, but larger insights are often revealed.
Artificial Intelligence won’t replace human investigators. Anyways, when used appropriately, AI can make investigators more effective.
Human capabilities are common sense, intuition, creativity. Together, experienced fraud investigators teamed with AI-capable anti-fraud technology are a yin-yang combination, each making the other perform better.